Other Surgical Options
There are a few options to consider in surgical weight loss. Every situation, individual, and health goals are different. Speak with your physician on the best options for your personal and health goals.
There are a few options to consider in surgical weight loss. Every situation, individual, and health goals are different. Speak with your physician on the best options for your personal and health goals.

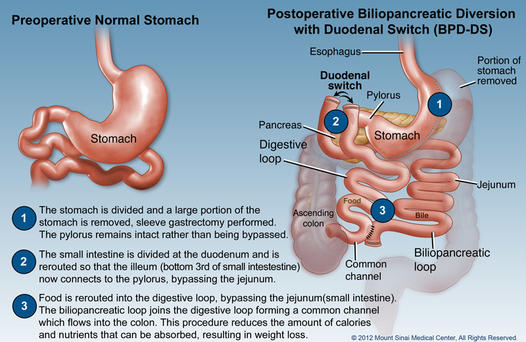
The biliopancreatic diversion with duodenal switch (BPD/DS) is a combined surgery that makes your stomach smaller and bypasses part of your small intestine for the best-reported, long-term percentage of weight loss. All insurance companies require a BMI of equal to or greater than 35 with co-morbid conditions, or a BMI equal to or greater than 40.
There are two parts to BPD/DS surgery:
The restrictive part uses a sleeve gastrectomy to make the stomach smaller while it works normally. The DS surgery keeps the pyloric valve intact, unlike other surgeries that bypass it. Keeping the pyloric valve intact lowers your risk of getting certain ulcers, or a blocked or narrowed opening (stoma).
The malabsorptive part of this surgery rearranges the small intestine to separate the flow of food from the flow of bile and pancreatic juices. This means you absorb fewer calories from most foods. Further down the digestive tract, the divided paths are rejoined. Food and digestive juices begin to mix, and some absorption happens in the common tract as the food continues on its path toward the large intestine.
Advantages of BPD/DS
After Surgery
The traditional duodenal switch with biliopancreatic diversion (DS/BPD) was first introduced in 1986. It is a complex bariatric surgery that has not been widely implemented despite its excellent results and long-term weight reduction success. Due to this a simple version of the duodenal switch was introduced over 5 years ago, the loop DS or the SADI. The SADI (single anastomosis duodenoileostomy) is a type of duodenal switch bariatric surgery that involves a loop anastomosis rather than traditional roux reconstruction. There are two parts to the surgery. First, a sleeve gastrectomy is made to reduce the size of the stomach. Second, the duodenum is divided just beyond the pylorus. The lower part of the intestine, the ileum is anastomosed to the duodenum at a length of 250cm from the terminal ileum. The bile and pancreatic enzymes will empty their normal route (afferent limb). Digestion of protein and fat now take place in a common channel. SADI is a new form of Duodenal Switch which has been around for just over 5 years. The fundamental differences between conventional DS and SADI are:
There is only one (1) with the anastomosis SADI compared to two (2) for the DS
With the SADI, there is a longest common loop through which nutrients pass, which causes a decrease in stool frequency, fewer side effects and less deficiencies in vitamins and minerals for the SADI compared to DS.
Advantages
Disadvantages
Risks
If you have had a gastric bypass, either laparoscopic or open and you were initially successful but now have experienced weight regain and are discouraged we are here to tell you there is hope for and there are options.
Often, the gastric pouch and opening to your intestine can be surgically revised. This can usually be done laparoscopically even if your previous surgery was open. Both your pouch and opening to your intestine (stoma) can be reduced in size so that you can re-lose the weight and comorbidities.
Dr. Domkowski specializes in revising gastric bypasses. Before your surgery we will need to perform some tests to understand your previous surgery, but they are done on an outpatient basis.
If you have had a previous gastric bypass, either open or laparoscopic, and have experienced weight regain and/or re-emergence of your diabetes, hypertension or obstructive sleep apnea you may be a candidate to have your surgery converted to a biliopancreatic diversion with a duodenal switch. This is a powerful malabsorptive procedure which should result in significant weight loss with elimination of your comorbidities.
Consider making an appointment with our bariatric surgeon to see if you are a candidate for this type of revisionary surgery.
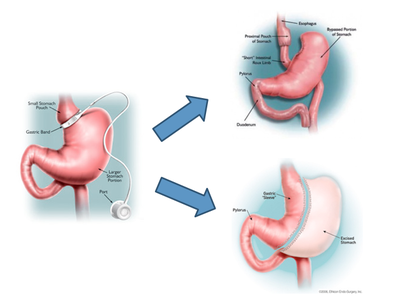
We no longer offer the gastric band at Steward Bariatrics & General Surgery, but if you have had a band placed and are experiencing problems we offer conversion of gastric band to sleeve gastrectomy or bypass.
Sometimes after people undergo gastric band surgery, they experience problems. These problems may include significant heartburn that does not seem to get better even with medication. They may also experience vomiting or difficulty eating despite being properly adjusted. This does not happen frequently, but when it does occur, it can be very frustrating. Alternatively, the esophagus (the tube above the stomach) may become dilated from the band being too tight for long periods of time. This is not a safe situation long term as it may lead to esophageal dysfunction or erosion of the band into the stomach.
Other potential but infrequent problems with the lap band include slippage or prolapse. That is the band changing position within the abdominal cavity. This may result in the band not functioning correctly and needing to come out. For those not wanting a replacement band, the laparoscopic sleeve gastrectomy may be an alternative option. Dr. Domkowski performs conversion of laparoscopic bands to laparoscopic sleeve gastrostomies and bypass.
Even if people have experienced significant weight loss with the laparoscopic adjustable gastric band, if it needs to be removed for whatever reason, then weight regain is highly likely. In order to keep this weight off long term, another bariatric surgery will need to be performed.
Both the laparoscopic sleeve gastrectomy and gastric bypass after lap band removal is a very good surgical option for many band patients who did not reach their weight loss goals. Early published data demonstrates excellent weight loss in those patients undergoing the laparoscopic sleeve gastrectomy and gastric bypass after removal of the gastric band.
If you are not happy with your laparoscopic adjustable gastric band, even if you had it placed in another state, please schedule an appointment today and be evaluated for the laparoscopic sleeve gastrectomy or laparoscopic gastric bypass.